Cancer and stroke NHS patients among thousands discharged with nowhere to live

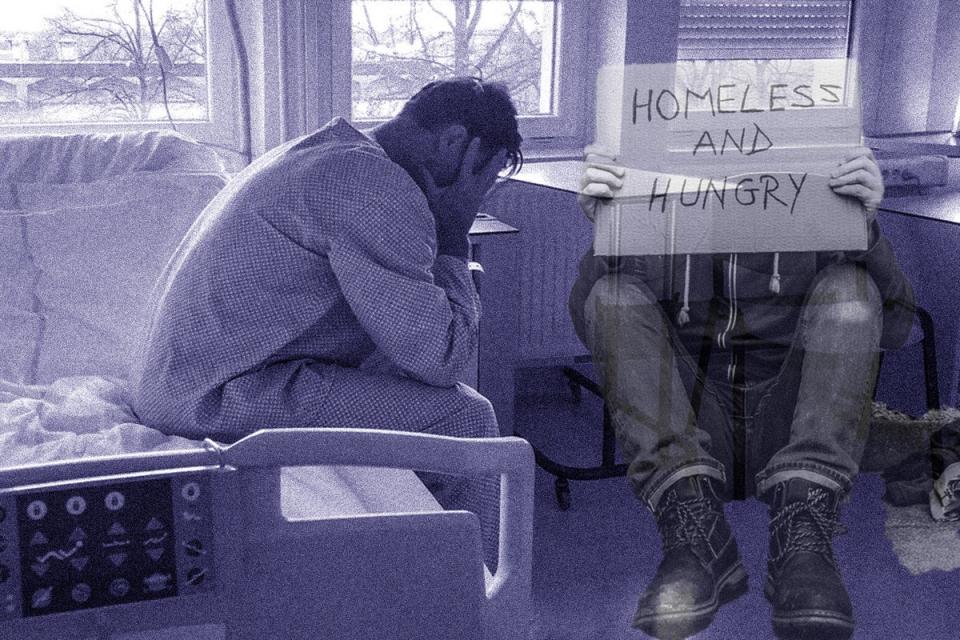
Cancer and stroke patients are among thousands of people being discharged from NHS hospitals every year with nowhere to live, The Independent can reveal.
People recovering from major surgery are also among those who have been released from care to “no fixed abode”, the designation for people with no home address.
In one instance, a man who had received surgery for testicular cancer three days earlier was left gripping a bag of morphine supplies and sheltering in a bus stop overnight as he worked out where he was going to live.
Hundreds of rough sleepers last year were found to have recently left hospitals, prompting MPs to call on the government to “break the link between rough sleeping and discharge from an institution”.
Those discharged to no fixed abode may end up in B&Bs, sofa-surfing or in temporary hotel accommodation after a recent hospital stay, while others may end up on the streets.
Charities called for an end to the discharge of hospital patients to the streets, warning: “We can and must do better.”
Nick Redmore, from the Salvation Army, responded to The Independent’s investigation, saying: “Despite the good intentions of hospital staff, these findings clearly show that, tragically, the system is failing patients who are homeless.
“Living on the streets, without shelter or washing and sanitation facilities, not knowing where your next meal is coming from and worrying about your safety, is no place for anyone, let alone someone recovering from illness or surgery.”
Shadow homelessness minister Mike Amesbury accused the Tories of “forcing more and more vulnerable people onto the streets of Britain”.
He said that a Labour government would ensure agencies worked together to stop “those at the sharp end falling through the cracks”.
Data obtained from around half of NHS trusts by The Independent shows at least 4,200 people were discharged to “no fixed abode” in 2022/23.
1,461 separate additional instances where people were discharged with nowhere to live were also recorded by trusts that year.
New data released by the government this month shows that 82 people, who had left hospital in England in the previous 85 days, were recorded as sleeping rough in December 2023. That number stood at 100 in October last year, figures showed.
Among the cases revealed in The Independent’s special report were:
• A man supported by the Salvation Army who told how he had been forced to spend a night on the streets after being discharged following a testicular cancer operation
• A woman who spent seven months in hospital with health complications after a fall, who had to live in a hotel for two months before she was helped to find a home by social enterprise tech company, Beam, which helps people crowd fund for financial support
• A charity worker who described seeing homeless people coming into a central London shelter with their hospital bands still on, needing urgent medical care because their health had deteriorated since they were discharged
• A man who had been sleeping on the streets of London, who said he felt he had been saved from death by an NHS trust who gave him a flat to recover in after his hospital stay
Recording a patient as having no fixed abode acts as a good indicator of the number of homeless people being treated but it is not a perfect record. Experts explained that some homeless people may give an incorrect address when asked, as they feel shame. They then won’t be recorded in the statistics. Similarly, some might be recorded as of no fixed abode if they came into hospital unconscious or in chaotic circumstances.
New research from charities Crisis and Pathway found that, according to more than 150 health service professionals surveyed, a shortage of council housing, NHS bed pressures and lack of care home placements are all contributing to the problem.
When asked, 13.7 per cent of health service workers said that patients were discharged to the street “all the time”, and 36.3 per cent said it was happening “often”.
Alex Bax, chief executive of Pathway, called for an end to “dangerous practices such as discharge from hospital to the streets”.
Matt Downie, Crisis chief executive, said their research had shown that “the availability of affordable, good-quality housing is fundamental to our health”. He added: “Westminster must work with NHS England to increase the availability of specialist care for people most excluded in our communities, to ensure no one is shut out from our healthcare system.”
Responding to this investigation, a government spokesperson said: “No one should be discharged from hospital to the streets”, adding that ministers were working “to make sure that people at risk of or experiencing homelessness have a place to stay.”
An NHS England spokesperson said: “All patients experiencing or at risk of homelessness should be referred to a care transfer hub, with clinical teams identifying at-risk patients as early as possible.”

 Yahoo Lifestyle
Yahoo Lifestyle 
